OCD and Autism: Understanding the Differences, Overlaps, and Support Options

Key Takeaways
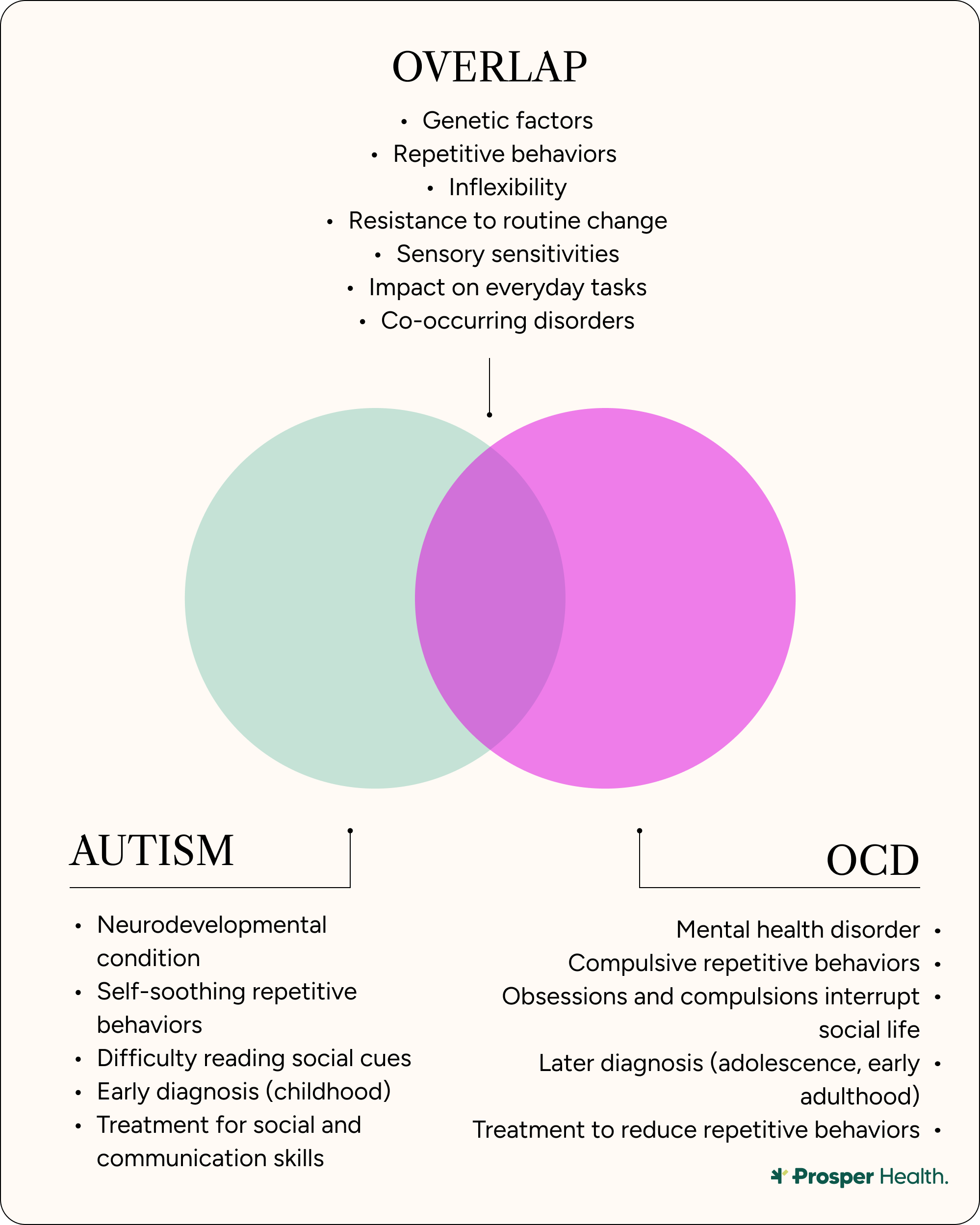
- There are many similarities between OCD and autism, including repetitive behaviors, inflexibility, and sensory sensitivities.
- Repetitive behaviors in autism are often self-soothing and regulatory, while in OCD, they are compulsions performed to reduce anxiety.
- Autism is classified as a developmental condition present from early childhood, while OCD is a mental health disorder that typically emerges in adolescence or early adulthood.
- Treatment goals differ, with autism treatment focusing on social and communication skills, and OCD treatment targeting repetitive behaviors to build distress tolerance.
- Therapies can be adapted for individuals with both conditions.
Having autism and obsessive-compulsive disorder (OCD) can be confusing for people with both conditions, especially because there are so many similarities between OCD and autism. It can also be a puzzle for people trying to figure out if they have autism or OCD.
However, overlapping traits, such as repetitive behaviors, can sometimes lead to an overall misunderstanding of the support people with these co-occurring conditions may need. This is mainly because although the characteristics of both autism and OCD are alike, the underlying reasons behind those behaviors are rather different.
As with autism, people with an OCD diagnosis are considered neurodivergent because they respond to the world differently than neurotypical individuals.
No matter where you are in your journey toward understanding OCD and autism (whether you’re considering an evaluation or have recently received a diagnosis), this article unpacks the differences between these conditions, as well as where they overlap. In addition, we’ll discuss understanding what it means to have both autism and OCD, as well as the supports available to you.
What is autism?
Autism spectrum disorder (ASD) is a neurodevelopmental condition that results in a difference in how one’s brain works, which ultimately shapes how autistic individuals interact with the world. This condition can affect how people communicate, behave, and process sensory information. It also impacts a person’s sensitivities to stimuli like tastes, sounds, and smells. An important distinction to keep in mind when discussing autism and OCD is that autism is not a mental disorder or mental illness.
Common characteristics of autism can include:
- Difficulties with social communication and interaction
- Restricted and repetitive behaviors, interests, or activities
This second characteristic, especially, is why determining the differences between autism and OCD can be so challenging: Repetitive thoughts and behaviors are common traits for both conditions, as well as strong reactions to sensory input, and difficulty adapting to change.
What is OCD?
OCD is a mental health disorder where people experience patterns of unwanted thoughts and fears. These patterns are referred to as obsessions. Having such obsessions can lead people to engage in repetitive behaviors or rituals, also known as compulsions. While compulsions are meant to reduce obsession-related anxiety, whatever relief they offer is usually limited. As a result, OCD-related obsessions and compulsions can impede daily activities and raise stress levels.
Some common traits of OCD can include:
Obsessions
- A fear of being contaminated by touching objects others have touched.
- Doubting that you've locked the door or turned off the stove.
- Intense stress when objects aren't orderly or facing a certain way.
- Avoiding situations that can cause perceived contamination, such as shaking hands.
Compulsions
- Hand-washing until your skin becomes raw.
- Repeatedly checking doors to ensure they're locked.
- Repeatedly checking the stove to make sure it's off.
- Counting in certain patterns.
- Arranging your canned goods to face the same way.
What do autism and OCD have in common?
While both OCD and autism are separate and distinct conditions, “they share overlapping features across biology, behavior, and daily functioning,” says Kristen Delventhal, LCSW, a psychotherapist and sibling to a woman with autism and OCD.
Similarities in genetic and neurobiological markers
“Both autism and OCD tend to run in families and are linked to differences in how certain brain circuits work,” says Ashley Peña, LCSW, the National Executive Director for Mission Connection. “Especially the parts that handle habits, flexibility, and problem-solving.”
Delventhal also notes that “there is some genetic overlap noted for these disorders.” Specifically, she names “variants in genes related to serotonin regulation, glutamate signaling, and synaptic development” as being “implicated” in both ASD and OCD. In addition, “dysregulation of serotonin and dopamine systems is noted in both,” while “glutamate abnormalities are also increasingly studied in both disorders.”
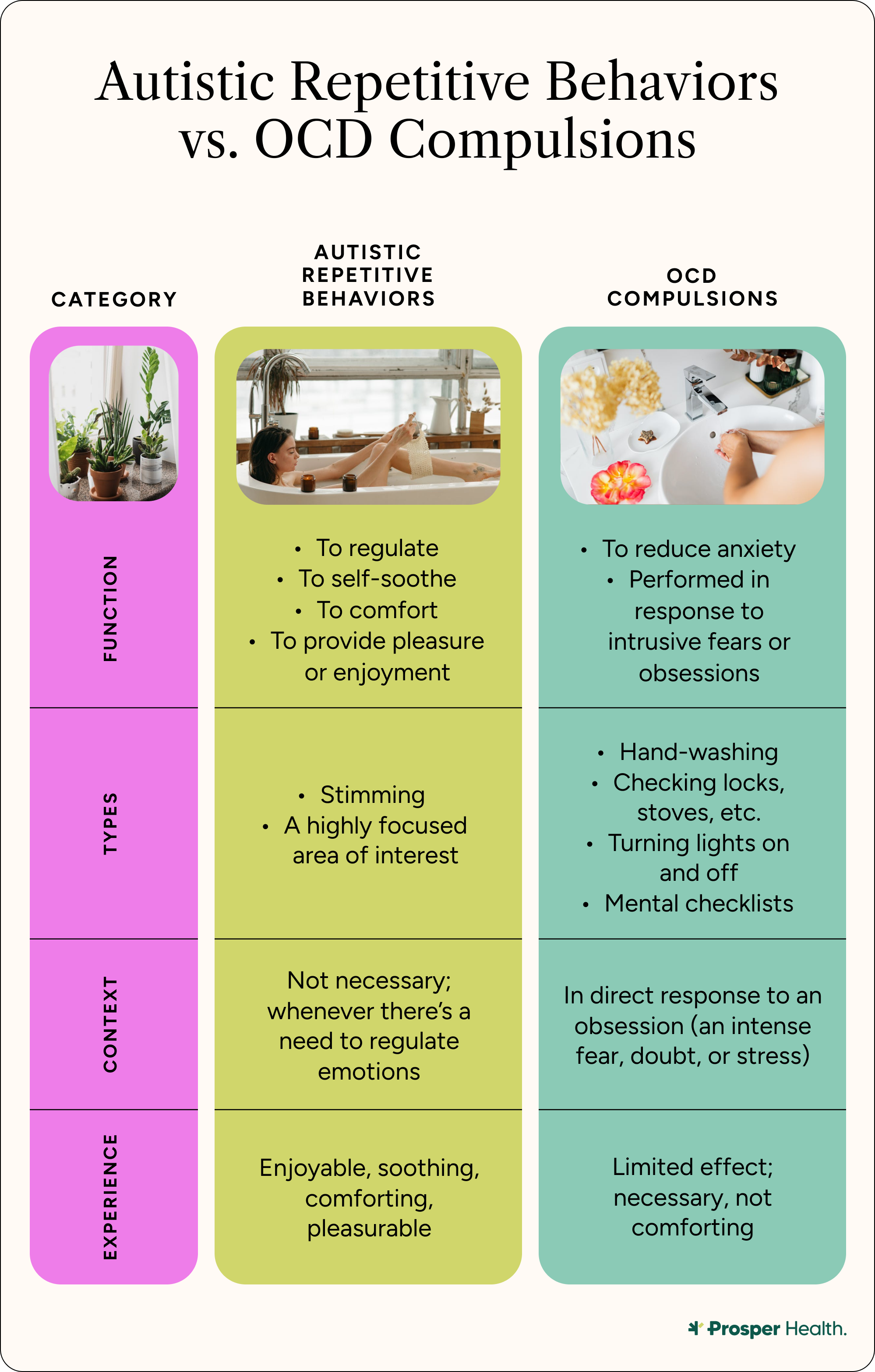
Similarities in repetition
As previously mentioned, repetition is a common trait of both autism and OCD, but Delventhal explains that this characteristic serves two entirely different purposes, depending on the condition.
“Repetitive behavior in folks with ASD is often self-soothing and regulatory,” she says, “such as hand flapping or lining up objects.” But for people with OCD, repetitive behaviors are “often related to compulsions that are ego-dystonic [ i.e., thoughts, impulses, and behaviors that are inconsistent with who we are] in nature.” Therefore, continues Delventhal, “folks with OCD do not find the compulsion inherently soothing, but necessary to reduce the anxiety they are experiencing.”
Still, people with both autism and OCD “can have heightened awareness and discomfort with sensory input, fueling repetitive behaviors,” she says.
Similarities in inflexibility
Inflexibility is another example of an OCD and autism overlap, as both conditions “can make it hard to shift routines or plans,” observes Peña. This can “lead to stress when unexpected changes happen.” And when stress is heightened, the co-occurrence of “rigidity, anxiety, and repetition can make functioning even more challenging,” says Delventhal.
Similarities in sensory sensitivities
Sensory sensitivities can present in either OCD or autism, though the reason differs by condition. “Many people with autism experience strong reactions to sights, sounds, textures, or smells,” says Peña. With OCD, however, these traits aren’t as straightforward: Peña acknowledges that “sensory issues are not a core part of OCD.”
But someone with OCD can still be sensitive to loud noises, and they can become dysregulated upon hearing a siren or fireworks. This can potentially cause the individual to engage in OCD rituals as a relief.
Similarities in the impact on functioning
“ASD often impacts social communication, learning, and independence, depending on the level of support needs required,” says Delventhal. Now, while “OCD does not inherently impact social communication or learning,” she explains that “the rituals and obsessions can impact access to learning and working.” These rituals and obsessions can also affect basic Activities of Daily Living, or ADLs (such as eating, sleeping, going to the bathroom, commuting, etc) due to the time needed to engage in them.”
In addition, OCD can have a significant impact on one’s social life since the rituals and obsessions can preclude spontaneity, as well as trigger anxiety around potential germs or contamination.
Similarities in the prevalence of co-occurring disorders
Not only are autism and OCD comorbidities, but both conditions also “commonly co-occur” with anxiety, ADHD, and depression, says Delventhal. “There is a wide range, between 10-30% of folks with autism or OCD who may also meet criteria for the other, based on a review of the research.” Since co-occurrence is common, Delventhal recommends “careful differential assessment and tailored treatment.”
How are autism and OCD different?
Noticing the key differences in OCD vs. autism can help avoid misdiagnosis, as well as delayed diagnosis.
Differences in classification
“Autism is classified as a developmental condition that is present from early childhood,” explains Peña, “while obsessive-compulsive disorder is categorized as a mental health disorder.” Both are usually lifelong conditions, but OCD traits can disappear and reappear over time.
Differences in repetitive behaviors
The repetitive behaviors that are present in both autism and OCD may appear similar, but “their underlying purposes are quite different,” emphasizes Peña.
“In OCD, compulsions are performed in response to intrusive fears or obsessions, serving as a way to reduce anxiety.” With autism, however, repetitive behaviors—such as stimming—“are often self-soothing, enjoyable, or connected to a focused area of interest.”
Differences in socializing
“Social functioning is another area where the two conditions diverge,” says Peña. “Autism directly affects social communication, often impacting the ability to interpret social cues, build relationships, and engage in reciprocal interactions.”
Now, while “OCD does not inherently cause these core social challenges,” the need to engage in compulsions can directly affect one’s relationships: “Individuals may experience disruptions in social life due to the time demands of rituals or the shame and secrecy surrounding their symptoms,” says Peña.
Differences in age of onset
“The onset of each condition also differs,” says Peña. “Autism is typically identifiable in the earliest stages of development, whereas OCD more commonly emerges later in childhood, during adolescence, or in early adulthood.”
Delventhal notes that “over half of OCD cases will occur before age 20.”
That said, while autism characteristics are often identifiable in early childhood, many children still go undiagnosed and may not learn they're autistic until they're an adult.
Differences in treatment goals
The treatment goals from an autism vs. OCD perspective vary, because OCD treatment tends to target repetitive behaviors, while ASD treatment revolves around social and communication skills.
“Treatment goals for ASD often focus on social skills, communication, and repetitive behaviors that are not necessarily restricted but instead shaped to be safe and reduce stigmatization,” explains Delventhal. This may involve therapies from CBT to DBT, mindfulness-based options, and more.
As for OCD, Delventhal says treatment does “target repetitive behaviors,” specifically as a way to help people “build distress tolerance around worry thoughts/anxiety thoughts and stop engagement in compulsive repetitive behaviors.” A common treatment is exposure and response prevention (ERP) therapy (more on that below).
Can autism and OCD co-occur?
Yes, it’s common for OCD and autism to co-occur since both are considered comorbidities, or coexisting medical conditions. However, the data for adults having both diagnoses is limited: One study found that 11.6% of autistic children and teens are also diagnosed with OCD.
However, these numbers are likely higher because only about 50% diagnosed with OCD present corresponding traits in their childhood or teenage years. The average age of OCD onset is 19, whereas “autism is typically identifiable in the earliest stages of development,” says Peña.
Diagnosis: How do clinicians tell the difference between OCD and autism?
Both conditions are diagnosed through comprehensive evaluations, with each evaluation looking at specific criteria.
How autism is diagnosed
Autism is diagnosed by either a psychiatrist, clinical psychologist, or neuropsychologist. The clinician will conduct several evaluations “that include developmental and medical history, behavioral observations, and standardized tests like the ADOS-2 (Autism Diagnostic Observation Schedule, 2nd Edition),” says Delventhal. These evaluations will also examine your social communication, interests and behaviors, habits, and day-to-day functioning.
An autism diagnosis is made when several criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) are met. They include:
- Social communication/interaction differences (all three required):
- Deficits in social-emotional reciprocity
- Deficits in nonverbal communicative behaviors
- Difficulties developing, maintaining, or understanding relationships
- Restricted/repetitive patterns (two or more required):
- Stereotyped/repetitive movements or speech
- Insistence on sameness or inflexible routines
- Highly restricted, fixated interests
- Hyper-/hyporeactivity to sensory input
Additionally, criteria must be met indicating developmental course—or evidence that these traits have been present from the early developmental period—as well as functional impact in day-to-day life.
How OCD is diagnosed
Like an autism evaluation, an OCD evaluation includes a thorough clinical and medical history. “Medical causes are always ruled out first,” says Delventhal. Then, the client is evaluated according to DSM-5 criteria, where clinicians look for the following:
- Obsessions, compulsions, or both
- If the obsessions or compulsions take up a lot of time (more than an hour per day).
- If the obsessions or compulsions cause distress or affect participation in social activities, work responsibilities, or other life events.
Some of the tools clinicians use to diagnose OCD include:
- Y-BOCS (Yale-Brown Obsessive-Compulsive Scale) – “considered the gold standard for measuring OCD severity,” says Delventhal.
- OCI-R (Obsessive-Compulsive Inventory – Revised) – a self-report checklist of symptom types.
Discerning between ASD and OCD
Generally speaking, clinicians can discern between autism and OCD when examining the reasoning behind certain behaviors: “If it’s to reduce anxiety, this typically leans more towards OCD,” explains Peña. “If it’s for comfort, enjoyment, or regulation, this would be indicative of autism.
“OCD behaviors usually feel unwanted or distressing,” she continues. “Autism behaviors often feel soothing or neutral.”
But there are also visible barriers that can affect one’s potential diagnoses. Specifically, masking (aka hiding their neurodivergent behaviors) and gender differences:
- Masking in autism: Many individuals mask their autistic traits for multiple reasons (wanting to fit in with neurotypical peers, hoping to avoid discrimination, etc.). They achieve their goal by mimicking neurotypical social behaviors, suppressing stimming, or forcing eye contact. Unfortunately, masking can impede any potential autism diagnosis, because this behavior “can hide core social-communication differences, making ASD less visible,” says Delventhal.
- Masking in OCD: Similarly, people who fear being shamed or judged may mask their OCD traits (performing their compulsions mentally instead of out loud, for example). But doing so “can downplay severity,” observes Delventhal, possibly leading to a missed diagnosis.
- Potential barriers: When people with autism and/or OCD engage in masking, “both groups may look ‘less impaired’ in structured clinical settings than in daily life,” says Delventhal. Since diagnoses rely on distinct criteria, hiding your true self during evaluations may cause more harm than good.
- Gender differences in autism: Girls and women are an underdiagnosed group because their autistic traits tend to fly more under the radar. Not only are they more adept at masking and social imitation skills, but their “special interests may be socially acceptable (e.g., animals, literature),” notes Delventhal. On the other hand, boys and men usually present “as more socially awkward or even hyperactive,” says Delventhal. This makes them less likely to mask—and therefore meet the DSM-5 criteria for diagnosis.
- Gender differences in OCD: Similarly, girls and women with OCD are more likely to avoid diagnosis due to “gendered social expectations,” says Delventhal. Since characteristics like “neatness” are more valued—and expected—in females, this can cause clinicians to sometimes normalize or minimize OCD traits. This could result in more missed diagnoses. Not an ideal situation, considering that women are at a greater risk of experiencing OCD in their lifetime than men.
- Potential barriers: Gendered social expectations can have a huge impact on potential diagnoses of OCD and autism. “This is when therapeutic rapport and having the skills to diagnose are vital to a clear differential diagnosis,” says Delventhal.
In addition to barriers like masking and gender differences, several other factors can pose a risk of OCD or autism misdiagnosis: First of all, Delventhal points out that “there is lots of misinformation out there.”
Plus, she notes that “not all clinicians trained in ASD will be trained in OCD, and vice versa,” which increases the risks of misdiagnosis or a missed diagnosis even more. Also, says Delventhal, “sometimes clinicians over-pathologize ASD traits as OCD,” while “OCD can be missed in folks with ASD, especially if they have limited verbal language skills.”
What supports are available for autism and OCD?
Seeking out support for OCD and autism in adults may seem like a gargantuan task, but rest assured, there are many options available that can be tailored to your particular needs.
A great place to start is by finding a neurodiversity-affirming therapist—a clinician who specializes in autism and/or OCD. They can help guide you through beneficial therapies and treatments with an understanding of your perspective.
Autism supports
For people with an autism diagnosis, both Delventhal and Peña recommend several different therapies, including, but not limited to:
- Speech therapy
- Occupational therapy
- Social skills training
- Mental health therapy
Some coping skills Peña advises include:
- Tools for sensory regulation
- Using alternative communication systems
- Building routines.
Delventhal also emphasizes the importance of community support networks for people with autism: “Adults with higher support needs may access supportive or 24/7 group home housing, day habilitation programming, and/or supportive employment.” Though she warns that the availability of these networks “varies widely by state.” In some states, she says, “there are limited adult services, waiting lists, and limited resources.”
And, due to budget constraints and Medicaid cuts, it may become harder for autistic adults to access these support networks.
OCD treatments and supports
There are two therapies that “are widely used to treat OCD,” says Delventhal.
- Exposure and response prevention therapy (ERP): This type of therapy “works on reducing compulsions and building the window of tolerance around this to work through and reduce anxiety,” says Delventhal. ERP, notes Peña, has “the strongest evidence base. Typically, 60-70% respond meaningfully, and, combined with medication, can enhance outcomes.”
- Inference-based cognitive behavioral therapy (I-CBT): This is a “cognitive-driven approach to working on addressing the thinking traps and irrational aspects of OCD that are reinforcing the compulsive behaviors,” explains Delventhal.
- Antidepressant medications like selective serotonin reuptake inhibitors (SSRIs): While Delventhal says that “medication can be used to ‘bring down the intensity’ around OCD,” it’s imperative to remember that “medication alone will not cure OCD.”
When both autism and OCD occur
While there are specific—and separate—treatments for autism and OCD, “therapies can be adapted to support the needs of folks with [both conditions],” says Delventhal. “For example, visual aids can be used more frequently with ASD-diagnosed clients. Pacing and predictability may be modified to support those with ASD as well.” She also emphasizes the importance of peer support for those who have both autism and OCD.
Here are some examples of modified treatments for both OCD and autism, courtesy of Peña:
- Adapted therapy: ERP and CBT can be modified with slower pacing, visuals, and clear steps.
- Sensory-friendly accommodations: Adjusting the environment (lighting, sound, texture) to reduce overwhelm
- Practical tools: Checklists, visual schedules, timers, and breaking down tasks
- Medication: SSRIs may still be useful, but need to be monitored carefully for sensitivity
How Prosper Health Can Help
If, after reading this article, you think you may be autistic, and/or have OCD, Prosper Health can help you find the support you need. Prosper Health provides telehealth autism assessments covered by insurance and specifically for adults.
Prosper Health can also connect you with neurodiversity-affirming therapy providers who specialize in autism and who can help you determine the right treatment path for all of your conditions.
- Diagnosis: Prosper Health offers telehealth autism assessments from clinicians whose specialty is working with autistic adults. And yes, many forms of insurance are accepted.
- Therapy: Prosper Health also provides ongoing, individualized support for autistic people through neurodiversity-affirming therapy. While working with Prosper Health, you’ll be matched with a therapist who will help you meet your goals and discover ways to thrive as a neurodivergent person.
Conclusion
Even though OCD and autism are two distinctive conditions, they’re similar enough to cause plenty of confusion, especially if you’ve been diagnosed with both! But no matter your diagnosis, both autism and OCD are valid experiences and manageable with the neurodiversity-affirming support.
“There are still a lot of misconceptions and stigma around ASD/OCD,” acknowledges Delventhal. “I am hopeful that the more we discuss both, the more we destigmatize and help educate the public.”
She also warns against the not-so-harmless habit of making “flippant” statements like ‘I am so-OCD,’” because they “can be harmful to those folks who are truly struggling.” OCD, like autism, is a very real medical condition, and should never be dismissed as a personal failing.
“With the right diagnosis and support, people with autism, OCD, or both can build fulfilling, meaningful lives,” assures Peña.
Frequently Asked Questions (FAQs)
Can you have OCD and autism?
Yes, OCD and autism are two different diagnoses, but it is common for people with autism to have OCD as well.
What are the differences between OCD and autism?
Autism is a developmental condition usually present from early childhood, while OCD is categorized as a mental health disorder. Another main difference between OCD and autism is the reasoning behind certain similar traits, such as repetitive behaviors or rituals. Repetitive movements, known as compulsions, in OCD, are performed to reduce anxiety. For people with autism, repetitive behaviors—like stimming—are a form of comfort or self-soothing.
What treatments work if I have both OCD and autism?
Several treatments for OCD and autism can be modified to help with both conditions. Therapies like ERP and CBT can be adapted for people with OCD and autism.
Can OCD look like autism?
Yes, especially when it comes to repetitive behaviors. This is why it’s so important to look at the reason behind these movements—are they in response to an obsession, or are they a source of comfort?
What percentage of OCD people have autism?
About 11.6% of autistic children and teens are also diagnosed with OCD. However, these numbers are likely higher because only about 50% of people diagnosed with OCD present corresponding traits in their childhood or teenage years.
What medication is used for OCD and autism?
Antidepressant medications like selective serotonin reuptake inhibitors (SSRIs) can be prescribed to help with intense OCD traits, but it’s important to remember that medication alone will not cure OCD. Therapy is one of the primary treatments for both OCD and autism.
Sources
https://pmc.ncbi.nlm.nih.gov/articles/PMC11048346/
https://health.clevelandclinic.org/understanding-ocd-and-autism
https://www.prosperhealth.io/blog/autism-and-stimming
https://my.clevelandclinic.org/health/articles/autism
https://lightonanxiety.com/what-are-ego-dystonic-thoughts/
https://my.clevelandclinic.org/health/articles/activities-of-daily-living-adls
https://my.clevelandclinic.org/health/treatments/25197-applied-behavior-analysis
https://www.mayoclinic.org/tests-procedures/cognitive-behavioral-therapy/about/pac-20384610
https://iocdf.org/about-ocd/treatment/erp/
https://www.prosperhealth.io/blog/special-interests-and-autism
https://www.prosperhealth.io/blog/neurodiversity-affirming-therapy
https://iocdf.org/ocd-treatment-guide/i-cbt/
https://www.mayoclinic.org/diseases-conditions/depression/in-depth/ssris/art-20044825
https://www.autismspeaks.org/advocacy-news/medicaid-cuts-coming-protect-autism-services
https://www.prosperhealth.io/blog/adapting-erp-therapy-for-autistic-adults
https://www.prosperhealth.io/blog/what-is-autism-spectrum-disorder
https://www.prosperhealth.io/blog/autism-masking
https://www.prosperhealth.io/blog/autism-vs-adhd
https://www.adult-autism.health.harvard.edu/resources/the-formal-diagnostic-criteria-for-autism/
https://embrace-autism.com/yale-brown-obsessive-compulsive-scale/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4530108/
https://my.clevelandclinic.org/health/diseases/9490-ocd-obsessive-compulsive-disorder
https://www.treatmyocd.com/blog/hiding-your-ocd-can-be-a-burden-heres-how-you-can-let-it-go
https://pmc.ncbi.nlm.nih.gov/articles/PMC3974607/
https://pmc.ncbi.nlm.nih.gov/articles/PMC6928520/
https://adaa.org/learn-from-us/from-the-experts/blog-posts/professional/how-sensory-processing-impacts-ocd
Related Posts

ADHD vs. Autism: Understanding the Differences and Overlaps
There is not a day that goes by that I don’t ask the question, “Is it ADHD or autism?”
As the parent of an AuDHD child—AuDHD being a colloquial term used to describe the dual diagnosis of both autism and ADHD—I still have difficulty differentiating between the two diagnoses. Is her stimming an autism or an ADHD trait? Which of her Individualized Education Plan (IEP) accommodations at school are tailored to her autism, and which ones are tailored to her ADHD? How is her ADHD medication affecting her autism traits?
My experience is with my 9-year-old daughter, but this dilemma is equally accurate for many adults. If you’re neurodivergent in any capacity, you’ve likely had moments where you’re comparing your characteristics, trying to determine if they could be a sign of autism, ADHD, or both.
AuDHD is becoming increasingly common among neurodivergent people, and those with both diagnoses deserve a clear understanding of autism and ADHD, and what it means when they co-occur.
That said, the two conditions are not the same! Many people will only get diagnosed with one condition or the other, so it's essential to understand how they differ.

Autistic Stimming: A Look Past the Stereotypes
Stimming, shorthand for self-stimulatory behavior, is a set of self-regulating behaviors commonly associated with autism spectrum disorder. Stimming can involve a wide variety of behaviors that stimulate one’s own senses, such as moving the body, playing with objects, or making vocalizations. Stimming, like many autistic behaviors, has been stigmatized, and often regarded as a symptom to be reduced by treatment. However, stimming is a normal, often harmless reality of autistic life, one that helps us regulate our senses and engage with the world more authentically.

Special Interests and Autism
Most autistic individuals have one or more special interests. A special interest is an intense fixation that far exceeds a typical hobby or passion. An autistic person will typically have the desire to devote large portions of their time, and sometimes large portions of their money, to their special interests. Neurotypical people can and do experience fixations or passions, but having a special interest is a trait strongly associated with autism.
Here’s what you need to know about special interests, how they manifest, the benefits of encouraging them, and more.
.webp)




